Infant Mortality Rate
An in-depth look at the infant mortality rate in Fort Worth in regard to zip codes

What to expect
Take a deep look into the infant mortality rate in Fort Worth in regards to zip codes. A study done from 2011-2014 by the University of Texas System states that although the state of Texas meets below the national average as far as infant mortality is concerned, certain zip codes within the city of Fort Worth are disproportionately affected. They go on to state, “For example, in Fort Worth, the infant mortality rate was more than six times higher in the 76164 zip code (12.3 deaths per 1,000 births) than in neighboring 76107 (1.8 deaths per 1,000 births).” What could be causing such a disparity, as well as possible solutions will be discussed.

What is infant mortality?
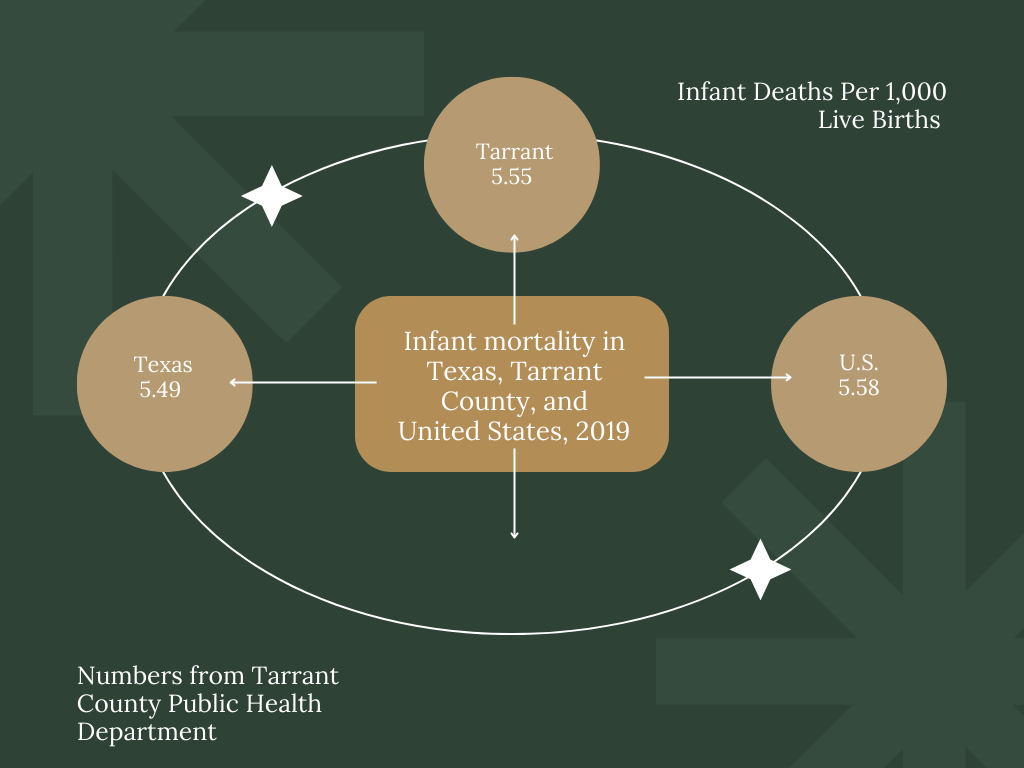
In order to take a closer look at this topic, it is important to have a basic, general understanding of what infant mortality is and how it is measured. It is also important to note that Tarrant County experienced its lowest ever recorded infant mortality rate back in 2019, right before COVID hit. An "infant," when looking at infant mortality rates, is a child from the moment they’re born to their first birthday. Any death that occurs within that first year is an infant death, thus making the term infant mortality. According to Kristin McElroy, the Maternal Child Health Epidemiologist for Tarrant County Public Health, these units are measured roughly every five years.
September is Infant Mortality Awareness month. Tarrant County's infant mortality rate fell to its lowest rate on record at 5.55 losses per 1,000 births in 2019. Expectant mothers and families are encouraged to look into the resources at: https://t.co/zM8Tb4WUtR. #infantmortality pic.twitter.com/HlnRHVVIAA
— Tarrant County Public Health (@TCPHtweets) September 14, 2022

Bigger picture
In the grand scheme of things, a large reason for the infant mortality issue in Fort Worth is due to a lack of resources, as well as differences in socioeconomic status. Radiance Women’s Health physicians assistant Tu Forkner said “typically, consistency in prenatal care and access to prenatal care is a big factor. Especially if, with Fort Worth, you're getting numbers from our county hospital. Over there, as well as in comparison to like Dallas, and Parkland here, a lot of patients end up not showing up until much later, they kind of miss a lot of their screenings."

The outside sign of the John Paul Smith Health Center for Women. (Tenae Durham)
The outside sign of the John Paul Smith Health Center for Women. (Tenae Durham)
“And so that tends to be a big issue. And sometimes even just kind of like transportation to stay really consistent with their OB visits as well. We see patients pretty consistently during the pregnancy, so every month initially, and then in the third trimester, you're here every two weeks, and then every single week towards the end. And so sometimes, if patients aren't prepared for that, that can also be a factor in staying consistent with their care," Forkner said. "Generally, at the beginning of pregnancy, we do a lot of screening for patients screening for hemoglobinopathies, IRA disorder, any STDs, STI, anemia, and things like that. So they get a pretty good sense of their health at the beginning of the pregnancy.
"But if they've missed some of that screening until later on, that can have a pretty big impact on the overall health outcomes.”

COVID
The effects of COVID and everything that comes along with it are still being discussed and studied. Especially how it may play out for new and expecting mothers.
“So far, I mean, we've seen some changes with a placenta. But I don't think there's anything that's been consistent so I'm not sure because we've had people that have gotten COVID have been okay, we've gotten some that have COVID and outcomes have been drastically different,” Forkner said.
So what could this mean for mothers in the future? The hope is to have greater understanding within the next few years. But with COVID there’s really no telling when to expect another update.
Fort Worth issue or something greater?
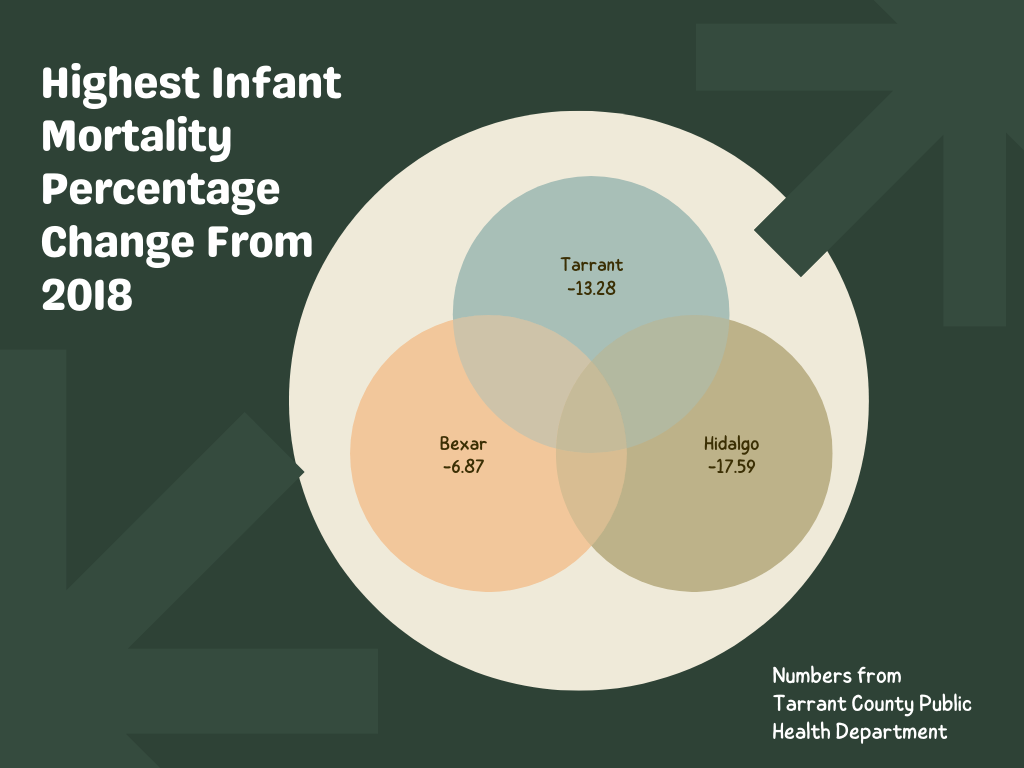
As stated previously, Tarrant County’s overall infant mortality rate went down and in 2019, was actually the lowest level ever reported. Forkner and the Mortality Review Coordinator for Tarrant County, Lauren Butschek-Neisler, both gave the same grim answer when asked if the infant mortality issue is a Fort Worth problem or a systematic one.
“I mean, it's probably a little bit of both, I think, you know, ease of getting to see a provider versus being able to take time off of work versus trying to find transportation. And then the financial costs of being able to come. I'm sure a little bit of both play into that as well. And kind of making it more accessible for patients,” Forkner said.
When asked the same question, Neisler said, “I think it's both. So our FIMR [Fetal and Infant Mortality Review] team looks at both local action, like things we can do within the county or the city to make changes, and also what can be done at a higher level. So systematically looking at you know, health insurance and Medicaid benefits and expansion and mental health access all those things at a higher level. But you know, at a local level, there are definitely things we can do. And some of those recommendations, we have looked like that as well. So I think it's a combination, it's not one or the other.”
If this is a city, as well as a systematic issue, it leads to the question of what could be done to alleviate the overall problem.

Where do we go from here?
What are the next steps? Now that the problem has been identified, what steps could be taken to help the women who are the most susceptible to these issues? Education seems to be the best place to start. Dr. Chao Li, the Medical Director of Maternal Fetal Medicine at John Peter Smith Hospital, as well as Forkner both agree that lack of education from the community on what steps to take, and reaching out to a healthcare provider later than what’s recommended are common issues.

Dr. Li working in his office. (Tenae Durham)
Dr. Li working in his office. (Tenae Durham)
“I think first, the patients need education. We need them to be aware there are resources they can seek, and that Medicaid is available for all the pregnant women. So they do have that resource. They need to see the doctor early, and that will establish prenatal care,” Li said.

The front door of the John Paul Smith Health Center for Women, where Di. Li works. (Tenae Durham)
The front door of the John Paul Smith Health Center for Women, where Di. Li works. (Tenae Durham)
Another thing that many aren’t aware of is the amount of resources that are available. Neisler even goes on to state, “I definitely think it can be resolved. And so part of the way, you know that, I think that it can happen. And you know, I've talked about it through local action. So our FIMR team is looking at case specifics, what's going on in our county, and what can we do, and they make recommendations to our Community Action Team. And that's where I think changes can be made. And we have multiple organizations and groups that come together, to review the data and review things that need to be changed and then take active part in creating that change.”
But if they could offer a piece of advice to the women most affected? "Find a provider you're comfortable asking questions with… And then take advantage of all of the pregnancy classes," Forkner said.
"So a lot of hospitals, especially if you're, you know, under the care of an OBGYN, will have access to baby classes and pregnancy classes… all of that is going to allow you to protect your baby in the womb and as they come out into the world.”



Photos Courtesy of Canva
